When we think of bone, we generally think of a skeleton, hard dead tissue. However, bone is a living, growing tissue made mostly of collagen. The human skeleton is the internal framework of the body.
Collagen is a protein that provides a soft framework, and calcium phosphate is a mineral that adds strength and hardens the framework. This combination of collagen and calcium makes bone strong and flexible enough to withstand stress. The bone mass in the skeleton reaches maximum density around age 21.
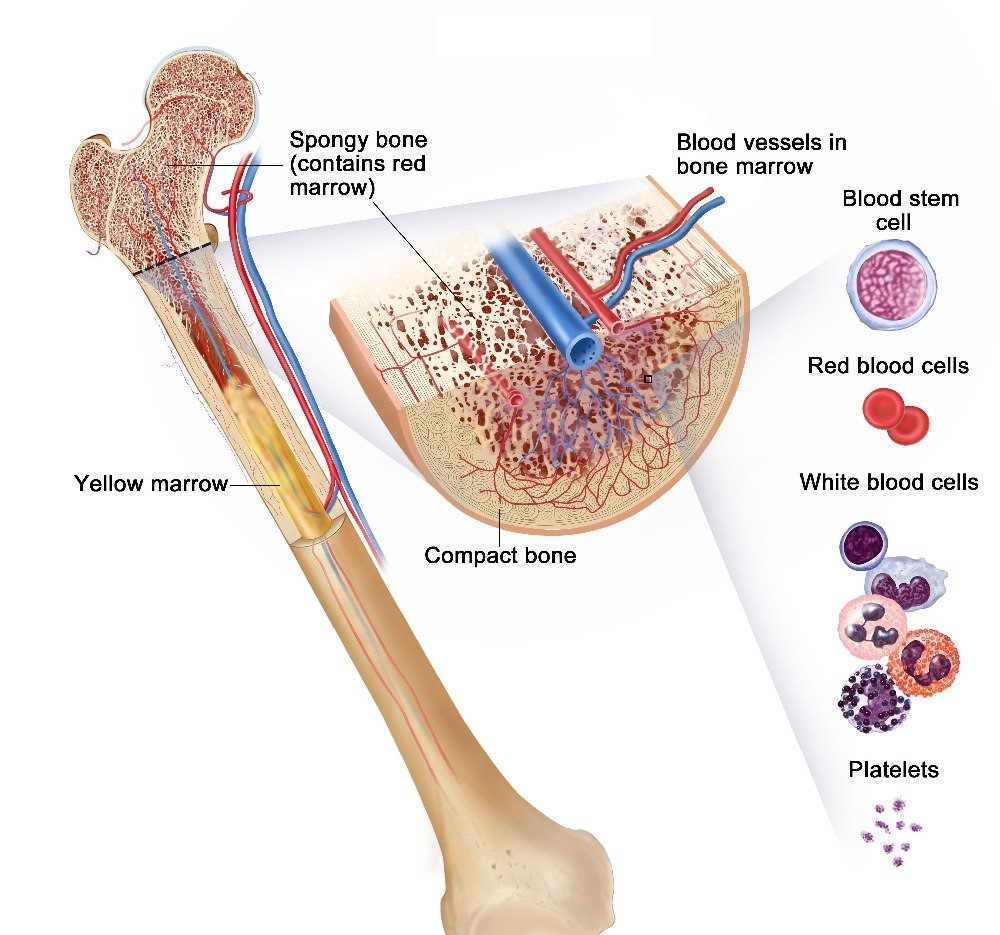
Bone marrow is the tissue comprising the center of large bones. It is the place where new blood cells are produced. Bone marrow contains two types of stem cells: hemopoietic (which can produce blood cells) and stromal (which can produce fat, cartilage and bone).
A fracture can be defined as a complete break in the continuity of the bone through trauma, which may be termed displaced or an undisplaced break. Classifications of fractures can be categorised into three groups depending on their aetiology:
- Fractures caused by a sudden injury/trauma, or high velocity impact.
- Fatigue or stress fracture, generally seen in young athletes.
- Pathological fractures – In the presence of disease i.e. cancer, tumours or osteoporosis.
Patterns of fractures
Patterns of fractures generally indicate the cause and will usually dictate the method of reduction.
- Transverse fractures – A transverse fracture through a long bone can be result of an angulation force.
- Spiral fractures – A spiral fracture is usually the result of high velocity twisting forces.
- Oblique fractures – An oblique fractureis a relatively common fracture in which the bone breaks diagonally.
- Comminuted fractures – These types of fractures are a result of compression or crush injuries and have more than two fragments.
- Impacted fractures – Where the bone fragments are forced firmly together that they become interlocked with no movement between them.
- Greenstick fractures – Occur in children and are common under the age of 10. They are ‘springy’ and resilient like the branches of a young tree. They tend to crumple like a concertina by longitudinal compression force.

The stages of fracture healing can take approximately 6 -12 weeks, which can be frustrating for an athlete wanting to return to sport. However, there are many factors that influence fracture healing, The age of the patient, the type of bone (cortical or cancellous), infection, or pathological changes.
Stages of fracture healing
A fracture will begin the healing process the minute the bone is broken, healing proceeds through many stages until the bone is consolidated.
1. Stage of Haematoma – The moment at which a bone breaks, blood will leak out from damaged vessels and forms a haematoma, (a solid swelling of clotted blood within the tissues.) The fracture inevitably divides the capillaries that run longitudinally in the compact bone.
2. Stage of subperiosteal and endosteal cellular proliferation – The most prominent part of the first stage of fracture healing is cell growth from the deep surface of the periosteum (a dense layer of vascular connective tissue enveloping the bones) These cells are precursors to osteoblasts (a large multinucleate bone cell which absorbs bone tissue during growth and healing). A collar of active tissue encircles the fracture site, bridges of tissue then grow towards each other.
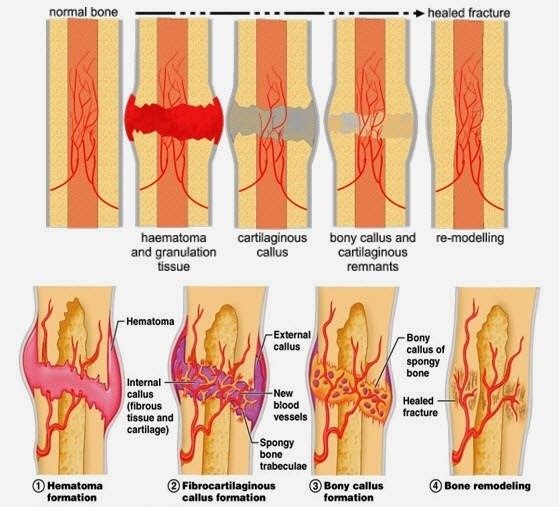
3. Stage of Callus – The osteoblasts lay down a matrix of collagen and polysaccharide, which soon become impregnated with calcium salts to form the immature bone of the fracture callus. This is termed as ‘woven bone’ which can be seen on x-ray indicating the fracture is uniting.
4. Stage of consolidation – The new woven bone which forms the callus over the fracture site, is gradually transformed into more mature bone with a typical lamellar structure.
5. Stage of remodelling – When union of the fracture is complete, this newly formed bone then forms a bulbous collar surrounding the bone. In the proceeding months the bone is gradually strengthened along the line of stress. This stage is happening continuously throughout life, although it becomes more evident following a fracture.

The above radiographs demonstrate a fracture at the point of break, right through the stages of fracture healing to bone union and remodelling.
How do we manage fractures?
The first management would be an assessment at A&E to establish if there is a fracture present. An x-ray will be performed to establish the nature of the fracture, which will subsequently determine the orthopaedic management. A conservative approach would be to reduce the fracture (align the bones) and apply a cast to fixate avoiding unnecessary movement while healing is taking place. If the fracture is displaced, an ORIF (open reduction internal fixation, pins & plates) may be required. Therefore, a surgical team will perform orthopaedic surgery. Part 2 will discuss Physiotherapy following a fracture, with progressive loading and return to sport.
Fiona Watson, Senior Physiotherapist
Physiohaus 2018


